Revenue cycle management (RCM) is a critical function in any healthcare organization. Unfortunately, the traditional RCM process is often manual, cumbersome, and time-consuming. This is where artificial intelligence (AI) can help. Reducing administrative costs, which account for over 30% of US healthcare costs, is a real opportunity for healthcare organizations to improve their financial success. Building and maintaining an effective revenue cycle requires experienced coders, meticulous documentation, and swift resolution of denials – all with the ultimate goal of managing expenses while providing quality care. It's not just about cost savings; it's about strategically structuring processes as part of overall organizational excellence. This is where artificial intelligence (AI) can help.
An autonomous medical coding solution with the right features can automate and streamline many of the tasks associated with RCM, making the process more efficient and effective. Here are four essential features to look for in a medical coding AI solution:
Autonomous coding is a requirement for modernizing the healthcare revenue cycle and will inevitably be adopted across the industry. Currently, claims data, most notably the codes within each submitted claim, are notoriously unreliable because it often lacks clinical specificity. Today, it is cost prohibitive to direct coders to spend extra time on each claim to apply standards above the fee-for-service bar of demonstrating medical necessity. From fee-for-service to population, organizations need a platform that is capable of removing the cost barriers to generate code sets with a high degree of clinical specificity with higher consistency and quality. By focusing on coding quality as a way to improve the quality of care and clinical outcomes while also reducing costs, healthcare organizations can realize unprecedented levels of value-based performance from their technology platforms.
Effective visibility and audibility of the decision-making processes are essential for trust in an AI platform. This can be achieved through transparent algorithms and timely reporting of revised decisions when data or circumstances change. Depending on the context, end-user stakeholders need to have access to code and explanations regarding how a system works, so as to understand the systems' reasoning, connections, and implications. Organizations should be able to monitor coding operations transparently and proactively, take corrective actions quickly, and be audit-ready at all times. Organizations should have access to a real-time analytics dashboard as well as evidence for every predicted code for every case.
Customers should be able to customize their experience exactly to their needs, enjoying a tailored service that is created specifically for them. Customers need the ability to tune and manage their systems to meet often unique and regularly changing requirements. This configurability should include quality and automation controls, configurable payor rules, organizational settings, and settings to enable predicted codes for unautomated cases to be visible to coders performing manual cases.
All health systems and provider organizations have made a significant investment in their EHR and the electronic workflow of their organization. Solutions should be designed to help customers leverage that investment by designing products to unobtrusively integrate into customers’ existing and future workflow.
According to SAP Insights, “A technology platform is the foundation for building and running business applications. The platform allows users to run their applications smoothly without worrying about the technology that supports them. At the same time, it allows technical staff to rapidly extend, enhance, or upgrade application software, increasing the speed of business.” Selecting a technology built on a platform is essential to ensure that the technology can be easily integrated into existing systems. Having a platform-based foundation allows for the potential to add more features and capabilities in the future, enabling healthcare organizations to quickly scale and adjust to changing demands.
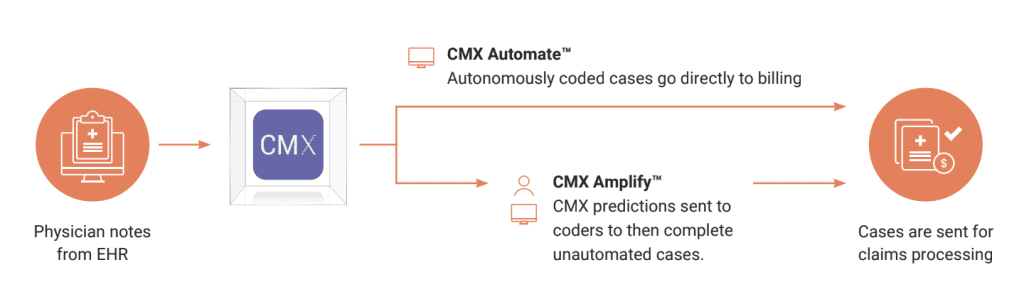
There are currently multiple autonomous coding solutions to consider, but only one provides all four of the above-listed features. CodaMetrix unlocks knowledge from the EHR and uses it to add value to healthcare providers. Our cutting-edge platform leverages artificial intelligence in the form of machine learning, deep learning, and natural language processing to continuously learn from and act upon the clinical evidence in the EHR. We automatically and autonomously translate clinical notes into billing codes that satisfy coding requirements, ensuring claims consistently represent the unique and complete episode of care while reducing the human coding workload.
From fee-for-service to population health CodaMetrix is focused on removing the cost barriers to generate code sets with a high degree of clinical specificity with higher consistency and quality. We invented the CMX Quality Rubric for quality classification of coding results, which our platform uses to extract coding best practices from a consortium of customers who choose to contribute their expertise and the “ground truth” data from their historical records. The CodaMetrix AI models deliver insights from coding best practices of highly regarded health systems in addition to applying each customer’s unique coding quality and compliance policies.Higher-quality coding results will be more effectively used by researchers and population health teams while improving patient care. Our focus on quality results in higher automation rates, lower denials, and significantly reduced costs.
CodaMetrix is designed for transparency from the ground up. The CMX platform is a glass box and not a black box. CodaMetrix customers have visibility into the CMX Dashboard for real-time analytics that displays the system's overall performance. Customers can view the percentage of automated cases versus manually coded cases in aggregate or by your defined organization. Automation results by case type like chest x-ray, mammogram, and CT are also available. Each case has a real-time case status with a final case resolution. Whether autonomously coded by CMX or manually coded by the customer’s coding team, the final codes assigned to the case are available for review and reporting on the CMX dashboard.The CMX platform provides evidence for every predicted code for every case. We provide case-level logic behind each predicted case with highlighted text corresponding to each predicted code.
As a provider-owned company, we understand revenue cycle management’s crucial role and how our customers need the ability to tune and manage their systems to meet often unique and regularly changing requirements. CMX codes autonomously, but our customers are at the helm. The CMX platform has many tools embedded to provide our customers with configurability. We provide quality and automation controls. Our customers participate in defining quality rubrics with us. Automation thresholds can be configured and changed to impact production within 15 minutes. We provide configurable payer rules, national and local edits, and customer-level rules. CMX is uniquely able to define and configure, on a per-customer and per-service line basis, what constitutes a case or a claim to be automated.
All health systems and provider organizations have made a significant investment in their EHR and the electronic workflow of their organization. The CodaMetrix solutions have been designed to help our customers leverage that investment by designing our products to unobtrusively integrate into our customers’ existing and future workflow. CMX AmplifyTM is a decision support tool that allows coders to work efficiently without needing to leave their EHR coding screens. This integration provides higher coding productivity rates with efficient tools.
If you're looking for an AI platform that has all of the must-have features for success in revenue cycle management, look no further than CodaMetrix. Our platform is designed with quality coding, visibility and audibility, configurability and control, and workflow integration in mind - everything you need to streamline your process and improve your bottom line. Schedule a demo today to see CodaMetrix in action and learn more about how we can help optimize your revenue cycle today.