“Any sufficiently advanced technology,” science fiction writer Arthur C. Clarke once said, “is indistinguishable from magic.” While Clarke wrote this in 1962, his idea has continued to resonate. These days, when we think about a technology that seems magical, one of the first that often comes to mind is artificial intelligence (AI).
At its most general, AI simply means getting a computer or machine to mimic the way humans think or speak. Out of the many potential applications for AI, there’s a good argument to be made that the healthcare industry has some of the most transformative. For instance, AI is currently being used to enhance surgical efficiency, improve diagnoses, and assist with medical research.
However, though they may seem less glamorous, administrative, operational, and revenue cycle tasks should not be overlooked when discussing AI’s applications in healthcare. Revenue cycle management is the process by which hospitals bill for services provided. It encompasses the entire lifecycle of a medical claim - from the time service is first provided to a patient to when that patient’s bill is paid in full. Patient registration, charge capture, claims submission, and coding are all part of the revenue cycle.
In many ways, coding is the lifeblood of hospitals and healthcare practices. It’s what turns services and procedures into billable revenue. It’s also the costliest and most manual process in revenue cycle management and requires highly-trained staff to comb through clinical notes and choose from tens of thousands of complex, nuanced diagnostic and procedural codes. Often, coders must seek clarification from physicians, which causes bottlenecks in the revenue cycle workflow and distracts from patient care. Further, organizations must contend with ever-raising rates of denials, which result in delayed (at best) or lost (at worst) revenue. Coding-related denials are among the most common and require significant staff resources to appeal and resolve.
Further, the healthcare industry is seeing a transformational shift from traditional fee-for-service (FFS) reimbursement models in favor of value-based care (VBC) models, which place emphasis on patient outcomes and care quality rather than the number and type of services provided. Proper documentation and accurate, thorough coding are essential components of VBC. “Coding with clinical specificity” ensures that the patient’s record has the most correct data which can then be used to improve population health initiatives.
Therefore, the value of AI cannot be understated. AI technology has the potential to mitigate many (if not all) of these stressors. AI can provide organizations with more efficient, accurate, high-quality coding, leading to increased reimbursement, reduced denial rates, an optimized workflow, less staffing burden, and less clinician oversight, which ensures physicians can remain focused on patient care.
“Physicians are our most expensive and scarce resource,” says Michael Mercurio, Executive Vice President of Strategic Partnerships and co-founder at CodaMetrix, and Vice President of Physician Revenue Services at Mass General Brigham. “AI can do the work they shouldn’t have to, so they can spend less time coding and more time caring.”
Therefore, not only does AI-powered coding automation have the potential to free clinicians from manual work so they can spend more time with their patients, as well as improve clinical decision-making, research, and population health; it’s also the first step to reimagining healthcare reimbursement models. Understanding these results, however, first requires a proper understanding of AI.
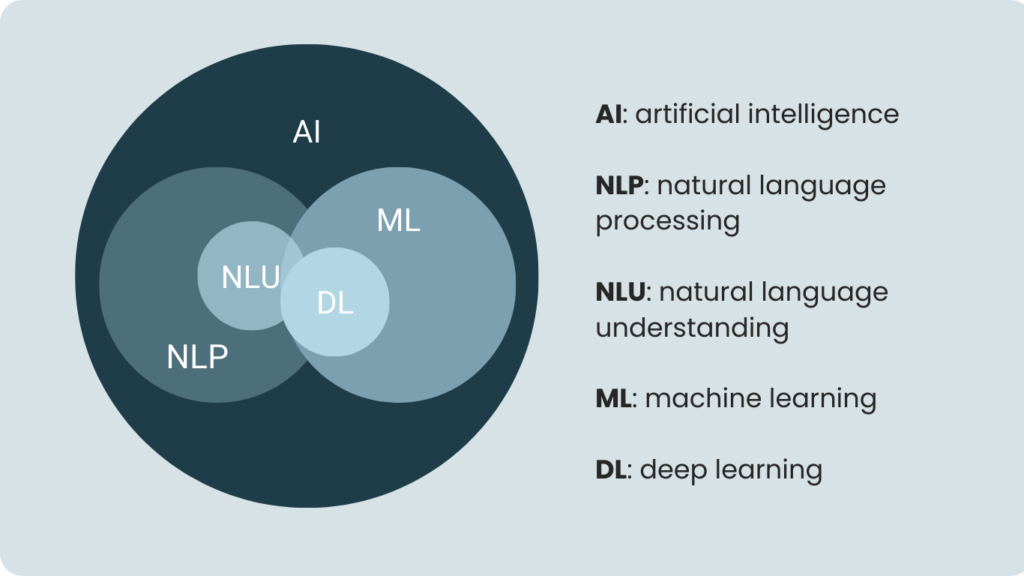
There are several concepts encompassed under the umbrella of AI application. Natural language processing (NLP) is the ability to process human language and identify keywords or phrases. Within this, natural language understanding (NLU) is the ability to actually assign meaning to these words or phrases. For example, NLP would be able to recognize “colonoscopy” as a statistically interesting phrase, whereas NLU will be able to actually define it as an endoscopic exam of the large bowel.
Standing alongside and enabling these concepts are machine learning (ML) and deep learning (DL).
“Machine learning is really about understanding patterns in data,” says Dr. Javed Aslam, professor at Khoury College of Computer Sciences at Northeastern University, ML expert, and CodaMetrix’s Chief Data Science Officer. “ML then uses those patterns to make predictions. It’s what enables AI to mimic human intelligence and ‘learn’.”
Without ML, AI would not be able to process or understand language. Taking it a step further, DL is a more powerful category of ML. It relies on neural networks, or vast arrays of processors that attempt to recreate the architecture of the human brain, in order to carry out complex tasks. This allows it to eliminate some of the pre-processing often required with ML and instead ingest and organize unstructured data.
The way these different concepts support and interact has given AI a wide range of capabilities across a number of industries. And just as there are a number of different types of AI, so are there a number of different ways to apply AI to the revenue cycle.
Let’s look at two of the most prominent approaches to using AI in revenue cycle management.
The first can be described as a “rules-based approach.” This relies predominantly on the natural language processing (NLP) component of AI to recognize certain words and phrases to assign them to the appropriate medical codes. For example, if the case documentation describes a “colonoscopy procedure,” the AI software would be able to automatically apply the appropriate CPT code as needed. The software will continue to analyze each word and phrase of the documentation to ensure all necessary codes are applied.
This approach is an important first step toward automating medical coding, but it has limitations. In order to know what code to assign to a given word or phrase, humans (often full-time medical coders or physicians) must first create a library of medical terminology and their associated codes for the program to use. With thousands of potential medical conditions, treatments, procedures, and code combinations, these rules can produce the same problems of manual coding: they are time-consuming and costly to produce. Even worse, they are difficult to transfer across organizations and specialties. If terminology differs, condition and treatment categories are not the same, [or the fields within the documentation are in different locations] then the rules “break” and must be fixed or created anew.
This is where machine learning (ML) comes in.
“In a traditional NLP/NLU-based system,” says Dr. Aslam, “someone has to manually craft and maintain the rules [that the system uses to code/is based on]. However, an ML-based system automatically learns the rules from data, and continues learning as it ingests more data.”
By using NLP and NLU to pull out [key/OR predefined] medical terms and phrases, an ML-based approach can analyze this data and then automatically create algorithms based on its confidence that a term corresponds with a medical code. If this likelihood is above, say, 95 percent, then the ML-based approach will assign the code. If it is below this confidence threshold, then it won’t. According to their needs, users can define how much they would like automated based on their desired confidence thresholds.
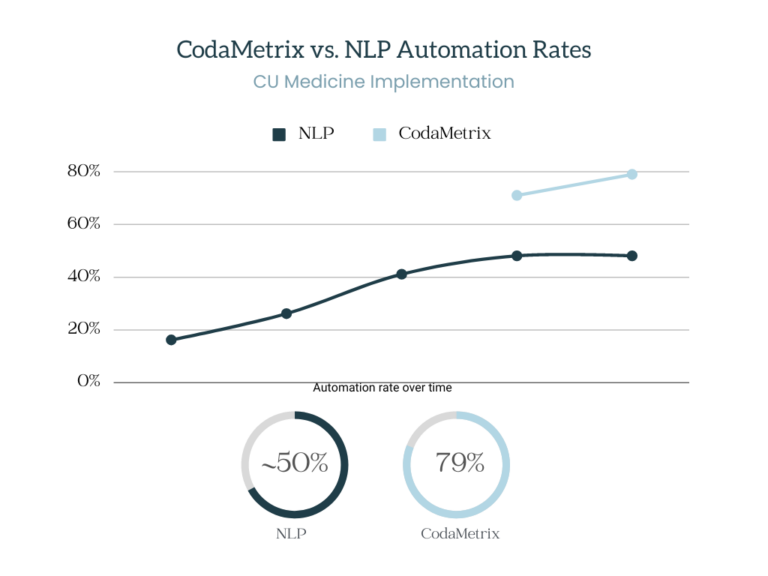
A key difference between NLP and ML is that while a rules-based approach can only be improved by generating more rules (and spending considerable resources to fix the ones that break), an ML-based approach will become more accurate over time by design. The ML-based approach to automating the revenue cycle is already proving its potential. Whereas an NLP-only approach plateaus at about a 50 percent automation rate (meaning it can automate any given medical case about half of the time), CodaMetrix’s own studies have shown that the ML-based approach can reach more than 70% percent automation rate. As more data is ingested, this rate continues to increase.
Additionally, the ML-based approach can drastically reduce coding-related denials. Denial rates are rising, and the reasons for denials are complicated and ever-changing. A recent study by Kaiser Family Foundation found that in 2020, insurers on the Affordable Care Act (ACA) marketplace denied nearly one in five claims on average, with claim denial rates ranging from 1% to nearly 80%! CodaMetrix’s research shows that ML-based autonomous coding results in 60% fewer denials than manual coding.
What’s more, the ML-based approach does not design rules around a singular specialty but instead builds one unified model that accumulates a variety of data across different specialties and can be applied to a range of different medical categories. As more users are added and more data is ingested, this model is able to learn more about how and when to apply certain codes. Whether encoding for radiology, pathology, surgery, GI special procedures, or another topic entirely, the accuracy rises as a result.
This blog only scrapes the surface of AI, ML, and how its various components can help modernize the healthcare revenue cycle. It’s an exciting field that will be critical for improving not just the efficiency and revenue of the healthcare industry, but for making clinical decision-making, research, and public health services as a whole more effective and reliable.
Read more about CodaMetrix’s AI-powered automation on our website.